All Graduates | 24 Jul 2019

Have you ever noticed how listening to audio-recorded content can make complicated ideas feel more accessible?
As it turns out, providing audio recordings to supplement written health materials may lead to better understanding and outcomes for patients. A study made in 2019 found that recording health education content in audio format, in addition to standard written materials, can improve patients’ comprehension and motivation.
The research followed two groups of culturally diverse Australians with chronic health conditions. One group received standard written education materials about their condition and treatment.
The other group received the same written information along with an audio recording of the content. The group with audio supplements reported a better grasp of the health concepts and felt more empowered to manage their condition. For patients with language barriers or learning challenges, audio content proved an effective way to boost engagement and understanding.
The implications are clear: if we want patients to get the most from health education, offering info in a mix of formats is key. When it comes to learning about health, hearing is believing.
Audio-Recorded Content Improves Discharge Instruction Comprehension for Limited English Proficiency Patients
Providing discharge instructions in a patient’s native language and preferred communication style is crucial for comprehension and adherence. A study named “Audio-Recorded Discharge Instructions for Limited English Proficient Parents: A Pilot Study” aimed to determine if audio-recorded discharge instructions improved understanding for patients with limited English proficiency.
The said study found that:
- Audio-recorded content in a patient’s native language increases comprehension of discharge instructions. Patients could replay the recording as often as needed to fully grasp important details about medications, wound care, diet, activity levels, and follow-up appointments.
- Both patients and healthcare workers reported high satisfaction with the audio-recorded content approach. Patients felt more at ease caring for themselves or their child at home, knowing they had a reference to return to if they had questions. Nurses appreciated that condensing instructions into a short recording forced them to focus on the most critical information.
- Providing real-time translation and recording was feasible but required adequate time. Occasionally, the process caused minor discharge delays. However, when successful, patients are left with a useful resource to share with other caregivers.
While the study was limited to a single children’s hospital and predominately Spanish-speaking families, the findings show promise for the approach. Prerecording standardized instructions and utilizing remote interpreters could help scale the intervention to more locations and languages.
 Overall, linguistically and culturally appropriate discharge instructions are vital for patient education and empowerment. For limited English speakers, audio-recorded content in their native language is an easy, inexpensive solution with significant benefits.
Overall, linguistically and culturally appropriate discharge instructions are vital for patient education and empowerment. For limited English speakers, audio-recorded content in their native language is an easy, inexpensive solution with significant benefits.
By ensuring comprehension, patients can properly care for themselves at home, follow up as directed, and stay out of the hospital.
By ensuring comprehension, patients can properly care for themselves at home, follow up as directed, and stay out of the hospital.
Study Tests Feasibility and Acceptability of Providing Recordable Cards With Audio Instructions
Recordable cards are a simple yet innovative way to provide language-specific discharge instructions to patients with limited English proficiency. A recent study tested whether these cards were helpful and acceptable for families after their child’s day surgery.
The study found that families loved receiving discharge instructions on recordable cards in their native language. Nearly half of families listened to the card more than five times, allowing multiple caregivers to understand the important details about properly caring for the child at home. Parents said the cards made them feel more at ease knowing they had the information they needed.
Providing the audio recordings in real time was challenging but feasible. Interpreters worked to efficiently translate the instructions into a 3-minute recording that was then reviewed with the family. On a few occasions, the process took too long for families waiting to be discharged, but usually, the cards were ready without delaying the discharge process.
The study was done at a single children’s hospital, mostly with Spanish-speaking families, so the results may differ for other populations. However, the overwhelmingly positive feedback shows that linguistically and culturally competent health care like recordable cards leads to increased patient satisfaction.
When patients can understand their discharge instructions, they are more likely to properly care for themselves or their children at home. Recordable cards represent an easy, low-cost solution to improve health literacy and outcomes. More research on their impact is still needed, but this pilot study suggests recordable cards in the patient’s language could reduce health disparities and benefit both patients and healthcare organizations.
The Majority of Patients Report High Satisfaction With Personalized, Audio Instructions
Studies show that when patients receive discharge instructions in their preferred language, they report higher satisfaction with their care experience. A recent pilot study found that most limited English proficient (LEP) parents were delighted with receiving personalized, audio-recorded content with discharge instructions for their child’s day surgery.
Over six months, researchers offered LEP parents either standard written discharge instructions or the standard instructions plus an audio recording of the instructions in their native language. Parents who received the audio recording were given a greeting card they could replay as often as needed to review the details of their child’s after-care.
Two to seven days after being discharged, parents were surveyed about their experience. Nearly all said the audio card was “helpful” or “very helpful.”
The study showed that this simple, low-tech solution empowered LEP families by overcoming language barriers and addressing health literacy issues. Parents felt more at ease caring for their child at home knowing they had the instructions at their fingertips in a familiar language and format.
While a larger follow-up study is still needed, these promising initial findings suggest that providing language-specific audio discharge instructions leads to greater patient satisfaction and comfort during recovery. For hospitals and healthcare organizations, this intervention could significantly improve overall patient experience scores and support better health outcomes, especially for culturally and linguistically diverse populations.
Audio Instructions Allow Patients to Review Key Information Multiple Times and Share With Other Caregivers
 Audio instructions allow patients and their caregivers to review key discharge information as often as needed. Rather than relying on written materials alone, an audio recording ensures patients fully understand what they need to know to properly care for themselves or a loved one once they leave the hospital.
Audio instructions allow patients and their caregivers to review key discharge information as often as needed. Rather than relying on written materials alone, an audio recording ensures patients fully understand what they need to know to properly care for themselves or a loved one once they leave the hospital.
As a patient, receiving audio instructions in your preferred language provides reassurance that you comprehend the necessary next steps. You can play the recording for family members and friends who will be helping with your recovery. Hearing the information aloud, especially in your native tongue, promotes understanding and allows you to ask any follow-up questions before you head home.
For healthcare workers, providing audio-recorded content or resources demonstrates a commitment to clear communication and the well-being of all patients, regardless of language or literacy level. Though time-consuming, recording instructions with the help of an interpreter builds trust and improves outcomes by lowering the risk of confusion or errors in aftercare. Patients who feel heard and cared for tend to have higher satisfaction with their experience.
While this study looked specifically at recordable cards for pediatric day surgery patients with limited English proficiency parents, the benefits of audio instructions apply to patients of all ages, languages, and medical needs. With advancements in technology and translation services, this simple yet impactful solution can be expanded to reach a larger audience, ensuring safe and effective discharges among diverse populations.
Overall, audio recordings lead to:
- Improved comprehension through repetition
- Increased confidence in managing aftercare
- Better continuity of care between providers and caregivers
- Higher patient satisfaction
By providing patients a voice, healthcare systems take an important step towards equitable, compassionate treatment for all. Audio instructions represent an easy, affordable way to dramatically improve outcomes and experiences. Though feasibility may vary, the rewards of overcoming any challenges are well worth the effort.
Implementing Audio Discharge Instructions Requires Planning But Shows Promise for Improving Outcomes
Providing audio-recorded discharge instructions in the patient’s preferred language is proving to be an effective way to improve health literacy and outcomes. A study found that giving Limited English Proficient (LEP) parents a greeting card with language-specific, audio-recorded content with discharge instructions for their child’s day surgery was feasible and led to high satisfaction.
This study aimed to determine if it was possible to give families these types of cards, see how they used and felt about them, and find out if the cards helped parents better understand the instructions and feel more at ease caring for their child at home. Parents with kids having day surgery between April and September 2016 could join the study.
Two groups were randomly divided: one received standard discharge instructions, while the other received the same instructions along with a three-minute audio card in their language for replay.
Two to seven days after leaving the hospital, parents did a phone survey. Those with the audio cards said they used them a lot, were happy to have them, and felt the instructions were clear and helpful. The cards let multiple caregivers get the details and parents could listen as often as they wanted.
While the study was too small to prove the cards improved understanding or comfort, the results suggest they have promise.
Providing real-time, language-matched audio discharge instructions is possible. Many hospitals have trouble translating medical instructions into other languages before patients leave. It often takes too long to translate everything accurately.
Not all medical centers have the resources to offer translations either. So some patients may leave without fully understanding their care instructions. Having interpreters record the instructions could be an easy fix.
For the study, it was key that interpreters had enough time to make and review good recordings and that families understood them. Most of the time, they made and explained the cards without delaying the discharge.
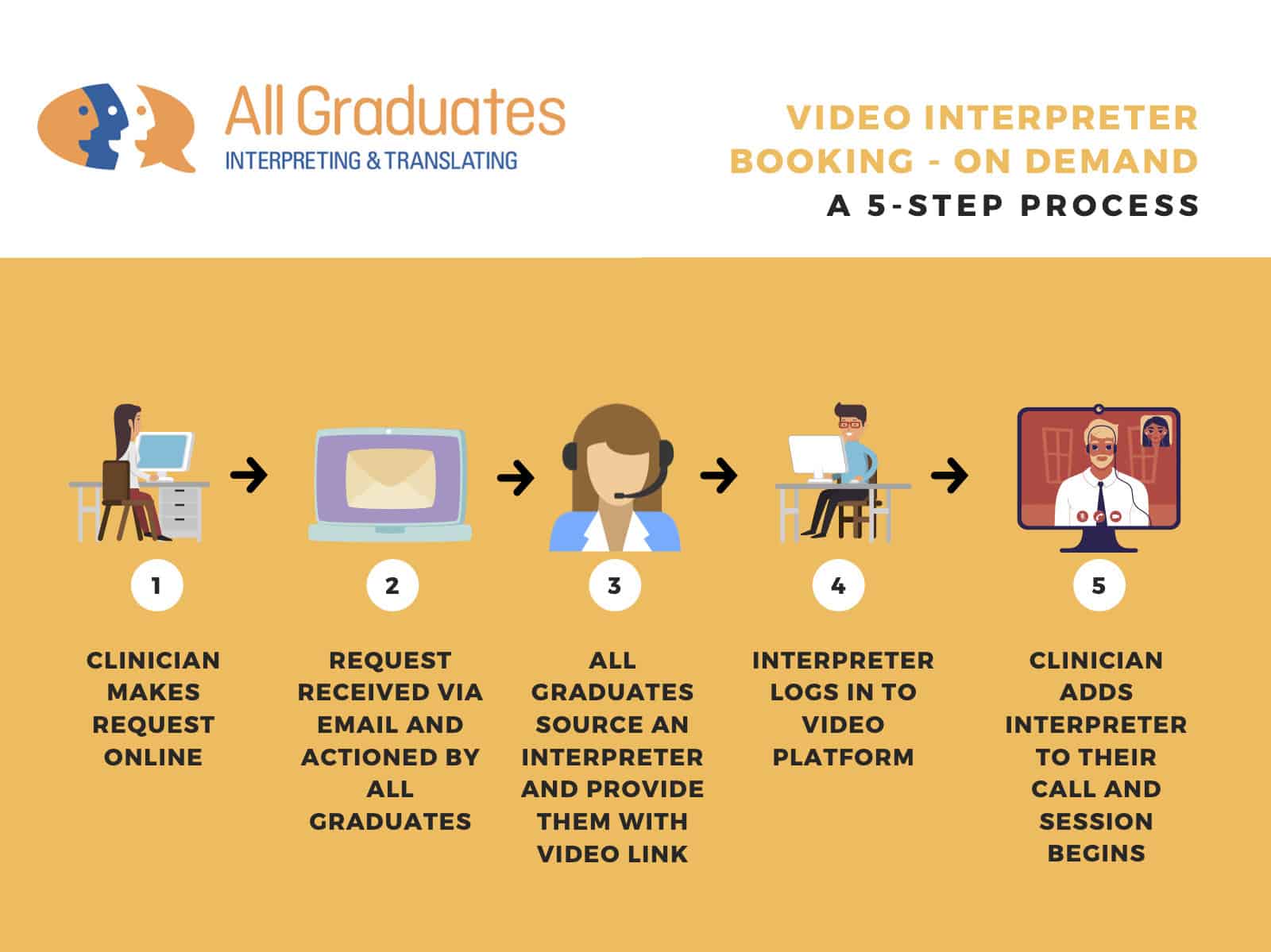
 This pilot study gives useful information for bigger studies on how to provide and assess language-appropriate discharge instructions. Options could include standardized prerecorded instructions and using phone or video interpreters.
This pilot study gives useful information for bigger studies on how to provide and assess language-appropriate discharge instructions. Options could include standardized prerecorded instructions and using phone or video interpreters.
The study found that recording discharge instructions in patients’ languages is a good idea. It helps make sure people facing language or reading barriers can still get important info they need before leaving the hospital.
Recording the instructions seems to work well and be a promising way to help communicate important time-sensitive details. Future research should explore their impact and usefulness for various groups.
Conclusion:
You’ve learned how recording patient conversations and sharing them can have significant benefits. Patients comprehend their conditions and care plans better when they review the discussed information. This leads to better compliance, follow-through, and health outcomes.
Healthcare providers also benefit from being able to listen back to consultations. When patients look over what was talked about, they can see where talking could get better. They may notice things they didn’t catch before. And they’ll have what they agreed on with the doctor written down to remember later.
Recording and sharing audio with patients can help both doctors and those seeking care. It’s an easy and affordable way for practitioners to connect with people and help them out. Win-win!
While change can be difficult, the advantages of this approach are clear. Patients experience a sense of ownership over their health journey. Doctors can have more effective and meaningful discussions. And the healthcare system as a whole benefits from better outcomes and reduced readmissions or errors.
If we want a patient-centered approach to medicine, audio content should be an essential component.
The future is calling – perhaps it’s time we start recording.
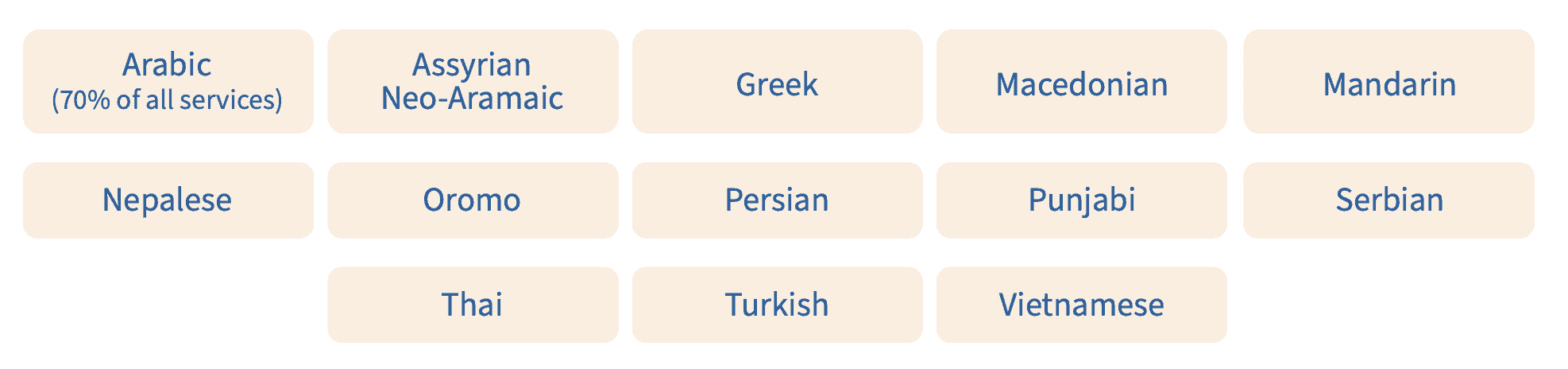
We, All Graduates, help doctors and nurses communicate better with their patients. Making sure healthcare providers understand their patients is important, no matter where they come from.
We’re experts in healthcare translation and are committed to patient-centered care. Let us be your partner in achieving better patient outcomes.
Contact us today to learn how All Graduates can help you bridge the language barrier and enhance patient care.
Read more: https://www.sciencedirect.com/science/article/abs/pii/S1553725018301600