Language is the link between behaviour and outcome

Ellias Appel | 25 Jun 2019
You’ve probably found yourself frustrated with how healthcare providers communicate. Maybe you felt like they were talking over your head with fancy medical jargon or not really listening to your concerns. The language used in healthcare settings has a huge impact on people’s experiences and outcomes.
When done right, communication can help build trust, convey empathy, and lead to better health for patients.
Unfortunately, too often language acts as a barrier rather than a bridge. This is especially true for marginalised groups who face discrimination and unequal treatment in healthcare. The words clinicians choose matter. Even subtle expressions can make certain groups feel excluded, disrespected, and less likely to seek care.
The good news is we all have the power to drive positive change through the way we communicate with each other. By making an effort to use more inclusive language, healthcare organisations and providers can help remedy inequities, break down barriers, and achieve the goal of providing the same high-quality experience for all.
In this article, we’ll explore some simple yet effective ways to get started. The path forward begins with awareness, empathy, and a commitment to do better.
The Role of Language in Healthcare
Inclusive language is essential for delivering equitable healthcare. It is the conduit through which understanding and positive behavior change can be achieved. Without effective communication, how can we expect to see the outcomes we desire, like reduced emergency department overuse or improved health literacy?
To start, the language we use must be engaging, accessible, and culturally appropriate. This means assessing both the level of English language proficiency and health literacy of our target audiences. This is especially important for health information, where misunderstanding the message can have serious consequences.
 Inclusiveness requires empathy. Our language should reflect an understanding of diverse experiences and perspectives. For example, avoid broad generalisations or terms that imply a single ‘norm’.
Inclusiveness requires empathy. Our language should reflect an understanding of diverse experiences and perspectives. For example, avoid broad generalisations or terms that imply a single ‘norm’.
Recognise and be sensitive to differing cultural attitudes around health, illness, and help-seeking behaviors. Promote shared values of access, equity, and empowerment.
Metrics provide evidence of impact, like increased knowledge, behavior change, or service utilisation. But behind the numbers, language plays a significant role.
It builds connection, conveys meaning, and ultimately determines whether we achieve our goal: improved health outcomes for all. Because when we get the message right, change will follow.
How Poor Health Literacy Impacts Outcomes
When patients have poor health literacy, it significantly impacts their health outcomes and the healthcare system. Studies show that those with inadequate health literacy have higher rates of hospitalisation and disease and lower life expectancy.
As a patient, not fully understanding health information makes it difficult to properly manage chronic conditions or follow treatment plans. This often leads to poor self-care and health choices. For the healthcare system, it burdens emergency departments and increases costs. According to research, emergency room visits can cost 4 to 14 times more than seeing a primary care doctor.
Poor health literacy also makes traditional health campaigns and education less effective for marginalised groups.
Some reasons for this include:
Language barriers: For culturally and linguistically diverse groups, language can be a major obstacle to understanding health information. Translating materials into other languages is not enough. The content and messaging must also be culturally appropriate.
Preferred learning styles: Different cultural groups may prefer receiving information in specific ways, e.g. oral vs. written. Audio and visual options should be offered in addition to the written word.
Power dynamics: Cultural beliefs about authority figures like doctors can impact how information is received and acted upon. Content should aim to empower patients and address any cultural taboos.
The good news is health literacy can be improved by making health information more accessible through:
Plain language: Using simple words and short sentences to explain medical terms and concepts.
Teach-back method: Asking patients to explain information back to you in their own words to ensure comprehension. Then re-teaching as needed.
Alternative formats: Providing information in audio, visual, and interactive formats in addition to text. It helps to bridge the gap between languages and cultures.
Cultural competence: Educating healthcare providers on cultural beliefs and learning styles of different groups to improve communication and trust.
With some adjustments to how we develop and deliver health information, we can achieve positive changes in health literacy and outcomes.
The key is making inclusive health communication a priority.
The Link Between Language and Behaviour
As a healthcare provider, the language you use has a direct impact on your patients’ behaviours and outcomes. The words you choose shape how your patients understand health issues and determine the actions they take.
Using inclusive, empathetic language can positively influence patients from culturally and linguistically diverse backgrounds, helping to improve health literacy and achieve better health outcomes.
Language Informs Thinking And Action
The language we are exposed to, especially as children, shapes how we think and behave. For CALD groups, limited English proficiency can limit health literacy and affect poor healthcare decisions. Providing information in a patient’s native language, or with the assistance of a qualified translator, helps to bridge this gap. It allows patients to fully understand their conditions and treatment options so they can make the best choices for their health.
An Engaged Patient Is An Empowered Patient
Taking the time to connect with your patients, understand their perspectives, and communicate in a meaningful way has significant benefits. Patients who feel heard and respected are more likely to follow recommended treatment plans and make informed choices. Engaging with patients from diverse backgrounds in an inclusive, culturally sensitive manner is key.
How can we improve engagement with diverse groups?
There are a few key ways to engage culturally and linguistically diverse (CALD) communities:
Use visuals: Images, videos, and infographics help overcome language barriers and improve understanding. Create simple animations to demonstrate health topics. Photos of people from diverse cultural backgrounds make your resources more relatable.
Provide translated materials: Offer resources in the languages of your target audiences. Ensure high-quality translations by skilled professionals.
Use audio: For those with limited English proficiency, hearing information can be more effective than reading it. Podcasts, videos, and phone messages are good options. Embed audio files that provide a translation of your written content.
Partner with community groups: Work with organisations that already engage your target audiences. They can help promote your messages and provide feedback on your approaches.
Train staff: Educate employees on health literacy, cultural competence, and effective communication across diverse groups. Their interactions and the language they use directly impact patient experiences.
The extra effort to positively impact the patient experience through empathetic communication and tailored resources leads to improved outcomes.
Metrics Matter
As a healthcare provider focused on outcomes and cost-effectiveness, the metrics matter. Non-critical use of emergency departments, for example, costs significantly more than primary care. For CALD groups, poor health literacy and limited English proficiency are often underlying factors in inappropriate Emergency Department use and other poor health decisions.
Providing information and resources in a patient’s native language has been shown to positively change behavior by helping patients better understand available health services and make more cost-effective choices. The investment in inclusive communication and culturally tailored resources can have a huge payoff, with some studies showing potential savings of up to 14 times the cost.
The link between language, thinking, and behavior is clear. Healthcare providers must make an effort to understand their diverse patient populations and meet them where they are. Speaking in a language they understand, providing information tailored to their needs, and engaging with empathy and care are some of the most impactful actions we can take to empower patients and achieve the best outcomes.
Improving Health Literacy in Diverse Populations
Improving health literacy among diverse populations requires strategic and thoughtful communication. Visual aids, like pictures and videos, can convey complex healthcare concepts when language alone may not suffice. Integrating literacy, culture, and language improves healthcare quality for all.
Meeting Diverse Needs
Different populations have different needs. Keep in mind that what is effective for one group may not be effective for another. Thus, one-size-fits-all solutions don’t always work.
Successful health literacy programs consider a community’s prevalent languages, cultural backgrounds, education levels, and more. They then develop materials suited to that audience.
For example, a program for new immigrants may provide information in multiple languages and use pictures to demonstrate key points. A program for elderly patients could have large print materials, and speak slowly and clearly while limiting complex medical jargon.
Culturally Competent Care
In order to achieve positive changes in healthcare, it is crucial to recognise the significance of providing culturally competent care to patients from diverse backgrounds. Culturally competent care refers to the ability of healthcare professionals to understand and respect the values, beliefs, and practices of different cultures, and to tailor their approach accordingly.
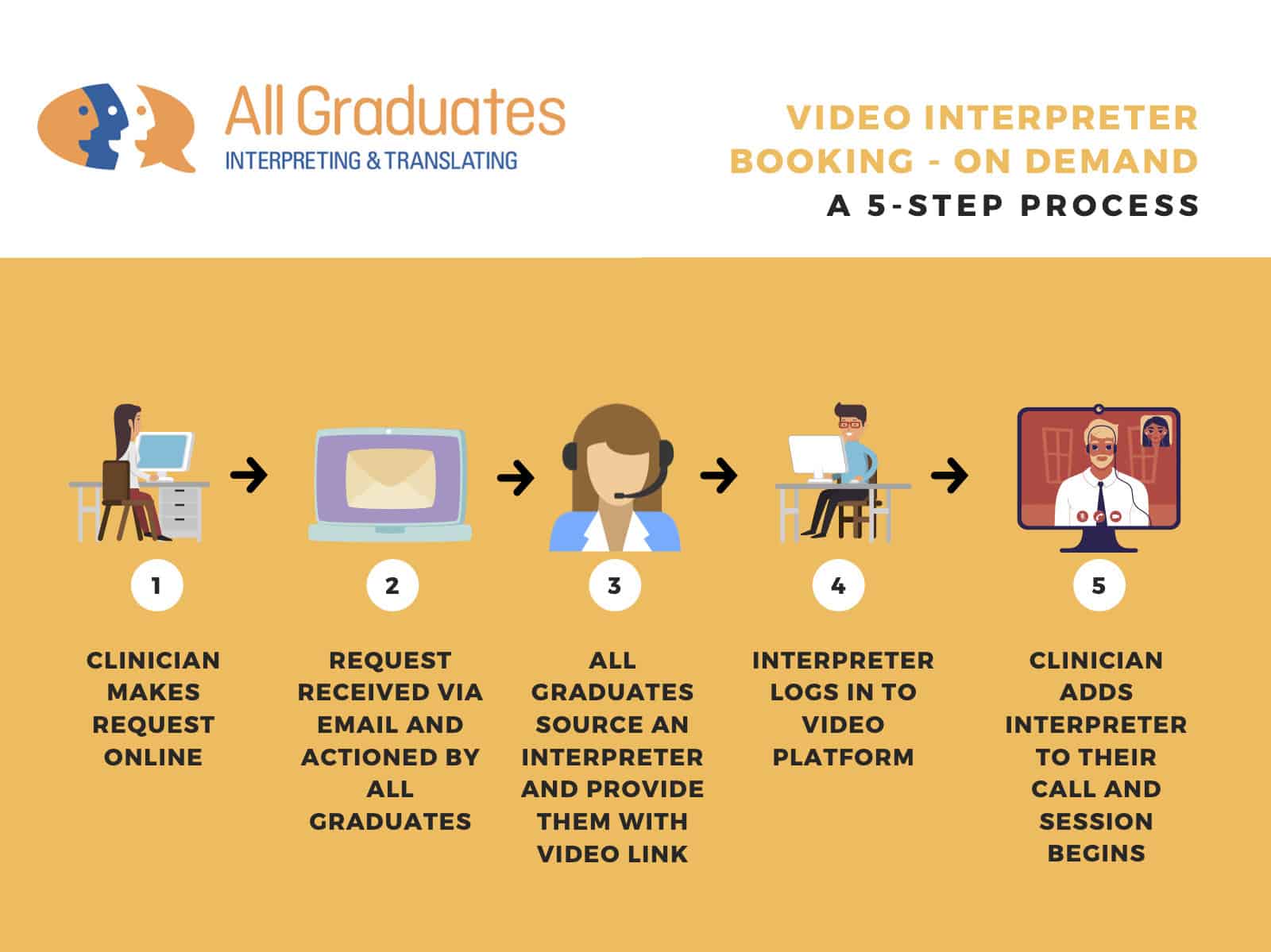
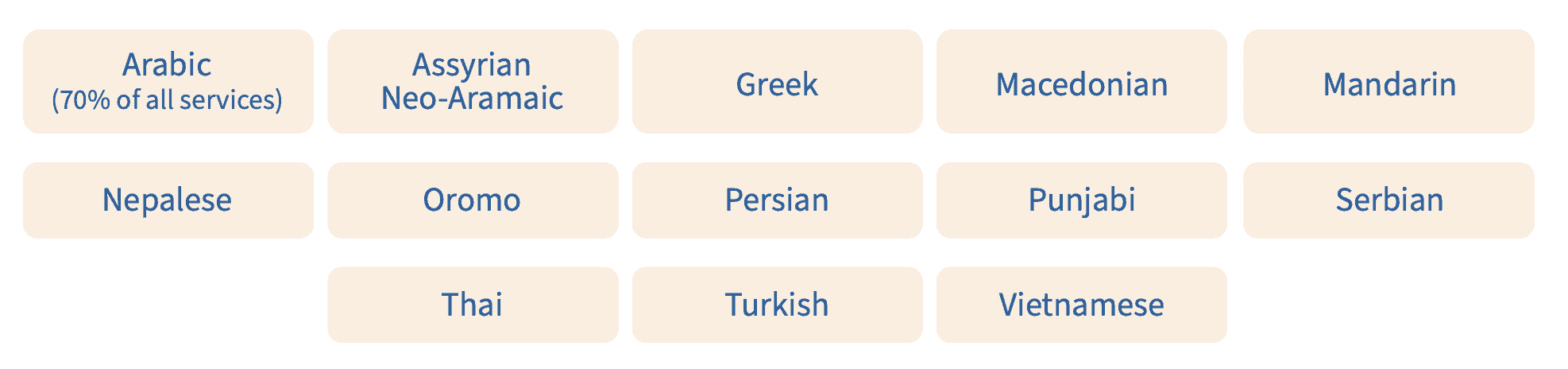
To ensure equal access to healthcare services, it is essential to offer language assistance options that go beyond just translations. Utilising trained interpreters (in-person or video remote) or telehealth services, providing audio translations, and employing culturally sensitive communication techniques can bridge the language gap and foster better understanding.
 Moreover, investing in health literacy initiatives for diverse populations can empower individuals to actively.
Moreover, investing in health literacy initiatives for diverse populations can empower individuals to actively.
By embracing cultural competence, healthcare providers can effectively address the unique needs and preferences of patients from various ethnic, religious, and linguistic communities. This not only enhances patient satisfaction and engagement but also improves health outcomes and promotes inclusive practices.
An Active Role in Health
Improving health literacy enables people to play an active role in their well-being. When patients are equipped with the knowledge and skills to understand medical information, ask pertinent questions, and adhere to treatment plans, they become partners in their own care. These lead to better outcomes and a more efficient healthcare system overall.
This collaborative approach not only leads to better health outcomes but also contributes to the overall efficiency of the healthcare system. By fostering a sense of ownership and empowerment, healthcare providers can create a patient-centered environment that respects diversity and promotes positive changes in healthcare delivery.
The bottom line: effective communication and culturally appropriate education are vital to improving health literacy in diverse populations. Using visual aids, simplifying language, and accounting for cultural differences are all strategies that make health information accessible to more people. And when people understand their health, they are empowered to pursue better well-being.
Creating Engaging Healthcare Content
To create engaging healthcare content for CALD communities, focus on using simple, inclusive language and an easy-to-understand format.
Think about your audience and what will resonate with them. Data suggests many in CALD groups face health literacy challenges and may prefer information in audio or visual formats. Provide content in the languages your audiences speak, and have it reviewed by native speakers to ensure it is culturally appropriate.
Keep it simple
Avoid complex medical jargon and aim for an 8th-grade reading level. Short sentences, bulleted lists, and double spacing will make your content more readable.
Focus on experiences
Help your audience relate by focusing on patient experiences. Share authentic stories of people from CALD communities using health services. Explain what to expect in a culturally sensitive way. This familiarises people with the health system and addresses fears they may have about accessing care.
Promote inclusiveness
Use inclusive and empowering language. Refer to your audience as “patients and community members” or “people” rather than labels like “CALD groups”. Explain that health services are for everyone, regardless of cultural background, language, or literacy level. Promote a sense of belonging and entitlement to use health resources.
Provide practical guidance
Give clear guidance on how and when to access health services. Explain the difference between emergency care, primary care, and after-hours options. Provide details on making appointments, bringing interpreters, and having a health care plan. The more people understand the health system, the more likely they are to use the appropriate services.
Using these techniques will help engage your CALD audiences and support them in making informed choices about their health care. The language and formats you choose are key to linking health messages to outcomes and behaviors. Crafting inclusive, empowering, and practical content can make a real difference.
Translating Materials for Inclusivity
 Translating materials into languages other than English is crucial for inclusive practice in healthcare. However, translation alone is not enough. To truly reach your audience and change behaviors, you need to consider how people from culturally and linguistically diverse backgrounds access and understand health information.
Translating materials into languages other than English is crucial for inclusive practice in healthcare. However, translation alone is not enough. To truly reach your audience and change behaviors, you need to consider how people from culturally and linguistically diverse backgrounds access and understand health information.
Simply translating written materials may not effectively engage these audiences or change behaviors. Partnering with community organisations and hiring professionals from diverse backgrounds will help ensure cultural appropriateness and relevance.
Consider your audience’s needs, values, and experiences.
What are the barriers preventing them from accessing the right care?
How can you empower them with knowledge and build trust?
What metrics will show your efforts are working?
Design materials and messages to be:
- Easy to understand, avoiding jargon and complex language
- Available in multiple formats (written, audio, visual)
- Culturally sensitive, free of assumptions, and inclusive of diverse experiences
- Accessible on mobile devices, public computers, and in community spaces
Continually evaluate your progress using real-world data and community feedback. Look for changes in behaviors as well as self-reported measures like awareness, attitudes, and satisfaction. When done right, inclusive health communication has the power to transform lives and strengthen our healthcare system. But we must go beyond translation to create meaningful change.
Using Data to Track Engagement
Using data to track how well your messages are engaging your target audience is key. As we explored in the previous section, language is the connection between what you want your audience to do and what they actually end up doing. To see if your approach is working, you need to monitor how people interact with your content.
There are a few ways to gather metrics on audience engagement:
- Trackable links: Create custom links for your content that you can use to see how many people click on them. Use a link shortener tool to create short, memorable URLs that redirect to your content. See which links get the most clicks to find your most popular topics.
- Download and interaction data: If you have digital content like audio files, videos, or interactive tools, see how often people access or use them. For example, track how many times an audio file has been downloaded or how long people spend using an interactive questionnaire.
- Surveys: Ask your audience directly how useful they found your content or resources. Surveys are a straightforward way to get feedback and see what’s resonating with people. Offer an incentive like a prize draw to increase the response rate.
- Social media: Monitor comments, likes, shares, and mentions of your content on social media platforms. See which posts get the biggest response to identify what your audience finds most engaging and interesting. Engage with people who comment to build goodwill and get additional feedback.
- Web analytics: Use a free tool like Google Analytics to get data on how people find and interact with your website. See how many visitors you get, what content they read, how long they spend on your site, and more. All of these metrics provide clues to what your audience finds most engaging.
 Using a mix of these data-gathering techniques, you can get a clear picture of how well your content and messages are resonating and make changes to improve engagement, especially for groups that face greater barriers. The more you engage your audience, the more successful your efforts will be in achieving the outcomes you want.
Using a mix of these data-gathering techniques, you can get a clear picture of how well your content and messages are resonating and make changes to improve engagement, especially for groups that face greater barriers. The more you engage your audience, the more successful your efforts will be in achieving the outcomes you want.
Evaluating Behavior Change in Patients
Evaluating behavior change in patients requires looking at metrics and outcomes. As a healthcare provider, you need to determine if your messages and resources are actually improving health literacy and achieving the outcomes you want.
For Culturally and Linguistically Diverse (CALD) groups, effective engagement often relies on addressing language barriers and cultural factors. Providing translated written materials alone may not be enough. Think about offering audio content, interactive options, and culturally appropriate translations. These can help bridge the gap for those with limited English proficiency or health literacy.
One study found that CALD patients were much more likely to inappropriately use expensive emergency department services for non-critical care, costing 4 to 14 times more than a primary care clinic visit. For these groups, poor literacy and English language skills can make traditional health campaigns less effective.
As an example, say you want to reduce non-urgent emergency department visits by increasing awareness of affordable after-hours clinic options.
How can you measure the resonance of your messages and the effectiveness of your behavioral change campaigns?
- Track referral links, IP addresses, and geolocation data to see who is accessing your audio or online resources. Notice any increases from CALD areas or communities.
- Survey patients at after-hours clinics to find out how they heard about the services. See if any mention your audio messages, translated materials, or website. Ask what was most helpful.
- Compare emergency department visit rates from CALD patients over time. Look for decreases that could indicate your resources are improving health literacy and behaviors.
- Get feedback from CALD community groups and leaders on the cultural appropriateness and effectiveness of your translated and audio materials. Make any needed changes.
- Consider doing focus groups with CALD patients to explore how your messages are received and see if there are any other barriers to behavior change that you could address.
Evaluating outcomes and making data-driven changes will help ensure your resources are achieving the positive impacts and behavior changes you intend for all patient groups. Providing inclusive, targeted options like audio and culturally sensitive translations is key to effectively engaging with and supporting CALD communities.
How will you know if your messages are resonating and behaviors are changing?
Conclusion
Language is a powerful tool that can be used to create and reinforce social norms, including those related to healthcare. Inclusive language practices can help to ensure that all patients, regardless of their background or identity, feel welcome, respected, and included in the healthcare system.
Something as simple as asking for a patient’s pronouns or avoiding insensitive language has the potential to make a huge difference in providing inclusive care.
In addition, it is important to be respectful of patients’ cultural backgrounds and identities. This means avoiding making assumptions about patients based on their appearance, accent, or name. It also means being mindful of the language that is used to discuss patients’ health conditions.
Speak up if you witness insensitive language, and lead by example using words that are inclusive, compassionate, and kind.
Achieving positive changes in language and inclusive practice in healthcare takes time and effort. However, it is essential to create a more welcoming and supportive environment for all patients.
Together, we can transform healthcare into an environment where people feel respected and cared for, regardless of their gender, background, or identity. Words have power, so choose them wisely and help create positive change.